
What is Periodontal Disease?
Periodontal disease is the inflammation and infection of the specialized structures that surround and support the tooth (gingiva, periodontal ligament, cementum and alveolar bone). By two years of age, 70% of cats and 80% of dogs have some form of periodontal disease.
Considering the dog and cat population in the United States extends into millions, this represents a huge problem. The diagnosis of this disease is oftentimes made late, as it is a quiet, insidious condition that doesn’t cause significant symptoms.
Commonly periodontal disease has been separated into two conditions: gingivitis and periodontitis.
Gingivitis is the term used to describe inflammation of the gums and is a reversible condition. Diligent home dental care is the single, most effective way to prevent the progression to periodontitis.
Periodontitis is the term used to describe the inflammation of the tissues supporting and surrounding the tooth, ultimately resulting in attachment loss. It can only be adequately diagnosed during an anesthetized intraoral examination along with diagnostic imaging: intraoral radiographs (X-rays) or CT. Periodontitis is irreversible but can be managed with professional periodontal therapies and diligent home care.
What Causes Periodontal Disease?
Periodontal disease is initiated by the build-up of plaque on the tooth surface. Plaque formation occurs in three stages. Initially salivary glycoproteins adhere to the tooth surface to form the pellicle. Pellicle is soft, and humans can recognize it as the substance that is brushed off the teeth or is removed during flossing. This substance is colonized by bacteria that find the perfect moist and warm environment for adhesion, followed by the third stage, maturation.
Once that biofilm is mature, very few things kill it. Plaque will eventually become mineralized by the calcium and other minerals in the saliva and form calculus (tartar). Calculus looks and smells bad, but it does not initiate periodontal disease. It offers a porous substrate for further bacterial adherence and continues to grow if not disturbed.
Signs of Periodontal Disease
The clinical signs of periodontal disease are subtle. Our pets are a big part of our family; very few people can resist big sloppy dog kisses! Most people would think bad breath (halitosis) is just “doggie (or kitty) breath”, but halitosis can mean more than that.
Other signs of periodontal disease can be noticed when looking at he teeth. The gums can be red and inflamed, teeth may look yellowish-brown, and the pet may be reluctant to have its mouth touched.
Oral pain is also common and can make a pet chew on one side, drop food out of its mouth, or have problems picking up the food. When the inflammation is severe, the gums can spontaneously bleed and traces of blood can be noticed in the water or in the food bowl.
In advanced cases, teeth will become loose and some can fall out on their own.
Understanding the Tooth Structure
To understand the development of periodontal disease, we have to first understand the structure of the tooth. In humans, dogs and cats, each tooth has one or more roots. In cats and dogs, incisors, canines and the first premolars are single-rooted, and the rest of the premolars and molars are multi-rooted. The gum (gingiva) surrounds each tooth like a turtle-neck collar.
Between the gum and the crown of the tooth, a space named the gingival sulcus exists. That sulcus is measured with a probe during professional periodontal therapy because its depth will inform the dentist of existing inflammation.
In patients with gum disease, the gingival inflammation will make the sulcus deeper and at that point, it is called a periodontal pocket. The bone loss due to periodontitis will expose parts of the root and the furcation.
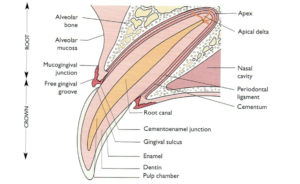
Figure 1. Structure of the tooth
The Problem with Non-anesthetic Dentistry
As previously mentioned, periodontal disease is the inflammation and infection of the structures that surround and support the tooth. The calculus visible on the crown of the teeth may look and smell bad, but it is harmless. The real culprit lurks in the gingival sulcus, so that is the area that needs to be addressed during professional periodontal therapy.
Non-anesthetic dentistry (NAD), also referred to as anesthesia-free dentistry, is a procedure in which the teeth are scaled and polished without the benefit of general anesthesia. NAD is considered not appropriate because of patient stress, injury, risk of aspiration, and lack of diagnostic capabilities.
Because a NAD procedure is intended to only clean the visible surface of the teeth, it allows the disease to progress below the gum line, while providing the pet owner with a false sense of benefit. It is very unfortunate when we see patients that had NAD in our office. Their owners have good intentions, they love their pet, and they think they are taking great care of their pet’s teeth! The reality couldn’t be further from the truth.
After years of anesthesia-free dentistry, the dog in this image lost so much bone structure due to undetected periodontal disease that it resulted in a grade 3 furcation exposure (the probe goes through the furcation area from one side of the jaw to the other).
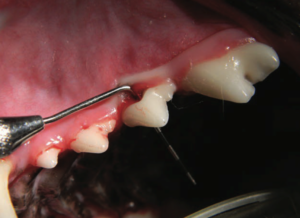
Figure 2 Consequences of NAD
Preventing Periodontal Disease
Creating a home dental care routine by brushing your pet’s teeth daily as soon as it is brought home, might be the single, most effective way to prevent this painful, debilitating disease. When recognized and addressed early, this is one of the very few diseases that is 100% preventable.
Several studies have proven that brushing teeth daily is the most effective way to prevent periodontal disease, making it the gold standard in home dental care. Other methods can be used like chews and drinking water additives, but none are as effective as brushing.
Brushing a pet’s teeth is a skill that requires some training. Cats may be a little more reluctant than dogs, but it can be done! A doggie or kitty toothpaste can be used, but it is not necessary. The mechanical action resulting in plaque removal is more important.
The training should be done gradually, over several days. You can start training your pet to accept having its mouth touched by first rubbing its lips, then lifting the lips and touching the gums. If you decide to use toothpaste, make sure it’s pet-safe and has a flavor you think your pet may enjoy.
Using a toothpaste in a flavor your pet likes will improve compliance. You can apply a little toothpaste to one tooth and let the pet taste it. When the touch and the paste are accepted, you can gradually increase the number of teeth and the amount on time you spend brushing.
It is not necessary to open the mouth, you only need to brush the outside of the teeth (the side facing the lips). To get further back in the mouth it may be helpful to pull the cheek out a little bit to make room.
The best scrubbing action would be provided by a soft-bristled brush (like a baby toothbrush) that is effective, but gentle at the same time. A wipe or cloth can also be used, but they will be less effective.
When finished you can offer a small dental-approved treat, and your pet will look forward to having its teeth brushed! In addition to all the health benefits, it will also improve the bond between you and your pet.
WATCH These Videos for Setp-by-Step Instructions on Pet Tooth Brushing
Treatment of Periodontal Disease
There are four stages of periodontal disease. This classification is made based on the extent of inflammation and subsequent loss of tooth root attachment and furcation exposure. The disease stage will influence the prognosis and treatment options.
Stage 1
For stage 1 periodontal disease, professional periodontal therapy is recommended every 12 months. As previously mentioned, it should be done in a veterinary office, under general anesthesia. Dental X-rays should be taken at every visit, as 30-50% of pathology can be missed if the roots are not imaged.
Power scaling, subgingival curettage and polishing should be performed by a trained professional. All other periodontal therapies start from the same basic procedure.
Stage 2
For teeth with stage 2 periodontal disease, after the basic cleaning, closed root planing is recommended. The root involved in the pocket is manually cleaned, and a perioceutic can be applied in the pocket. The perioceutic is an antibiotic gel that will occupy the space, fight the bacteria and the harmful enzymes they produce, and so reduce inflammation.
The body will have a chance to heal and the side of the pocket may be reduced. The follow-up periodontal therapy may be recommended sooner to assess the results (in about 6 months).
Stage 3
For teeth with stage 3 periodontal disease, the pockets are very deep, and can only be cleaned effectively by doing open root planing. This is a surgical procedure that creates and elevates a flap of gingiva to allow proper visualization and cleaning of the root.
Further treatment to promote attachment can be done using guided tissue regeneration. A particulate bone graft is placed in the pocket, covered with a bone membrane and the gingival flap is sutured back over the area. The recommended follow-up for this procedure is 3-4 months.
Stage 4
Teeth with stage 4 periodontal disease have advanced attachment loss and usually need to be extracted. In select cases involving a multirooted tooth, where only one root is affected by periodontal disease, we can perform a hemisection of the tooth.
The sick root is extracted, and the healthy one will receive root canal therapy and be saved.

Figure 3. Picture of the right maxilla of a dog showing teeth with advanced periodontal disease. Note the advanced calculus and severe gingival inflammation.
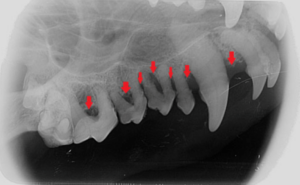
Figure 4. Radiograph of the right maxilla of the same dog as in Figure 3 with advanced periodontal disease. Note the severe bone loss (>50%) and furcation exposure.
Consequences of Untreated Periodontal Disease
The attachment loss that is caused by advanced periodontal disease will lead to loss of teeth and loss of bone. The disease is more common in small breed dogs, and the loss of bone is more dramatic in their fragile jaws.
Pathological fractures of the mandible and development of an oronasal fistula (communication between the mouth and the nose) are frequent sequelae of bone loss.
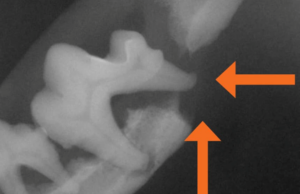
Figure 5. Pathological mandibular fracture due to catastrophic bone loss caused by advanced, untreated periodontal disease.
Vet Dentist in Phoenix
Regularly brushing your pet’s teeth is the gold standard of at-home dental care. Daily brushing in addition to dental treats and other oral health practices will go a long way in preventing gum disease. If your pet is in need of a dental cleaning, contact us at Carefree Dentistry and Oral Surgery for Animals.
Photo by Priscilla Du Preez on Unsplash
